New Born Screening: Data from India
In India, the prevalence of inborn errors of metabolism (IEM) is one in 2497 newborns and in Andhra Pradesh, one in 1000 newborns.
(Verma IC. Indian J Pediatr. 2000;67:12.)
(Ramadevi AR, Naushad SM. Indian J Pediatr. 2004;71:157.)
A paper collating a study conducted in four major Government Maternity Hospitals in Hyderabad shows incidence of Diseases as follows:
Metabolic Disorder Screened: Incidence
Amino Acid 1:3600
Phenylketonuria 1:18300
Transient Tyrosinemia 1:9000
Hyperglycinemia 1:18300
Hyperargininemia 1:18300
Congenital Hypothyroidism (CH) 1:1700
Congenital Adrenal Hyperplasia (CAH) 1:2600
Galactosemia (GALT) 1:10300
G6PD 1:2200
Overall Incidence Rate 1:540
A paper presents the results of a study done at KEM Hospital in Mumbai from 1978 to 2004. The following data is estimated incidence for 24 Million babies born in India.
IEM: 1: 1300
Sickle Cell: 1: 5100
(Inborn Errors of Metabolism (IEM) – An Indian Perspective, N. B. Kumta, IJP, Volume 72, April 2005. )
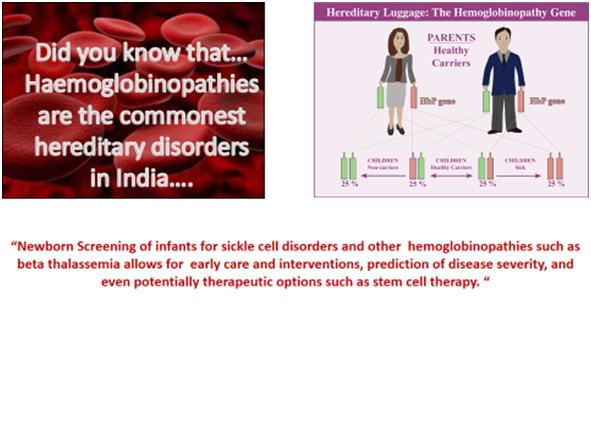
In a large Multicenter Study, the prevalence of β-thalassemia varied from 0 to 10.5 % among the different caste/ethnic groups and the prevalence of HbE trait varied from 0 to 66.6 % in the two eastern and north eastern cities.
J Community Genet. 2013 January; 4(1): 33–42. Prevalence of β-thalassemia and other haemoglobinopathies in six cities in India: a multicentre study D. Mohanty, et al.
The success of prevention programmes for the control of thalassemias in countries like Cyprus, Italy and Greece have shown that education and screening forms the most important part of these programme.
Specimen Collection Guidelines & Reports
Specimen Collection Guidelines
Accurate specimen collection is a vital step in the screening process. Please review the guidelines to ensure your sample is collected and submitted correctly.
- Specimens should be collected at the same time as the specimen for state mandated testing. The ideal time for collection is between 24-48 hours of age.
- If the newborn is discharged before 24 hours of age, a repeat specimen should be collected at about 48 hours of age from the pediatrician. Critically ill newborns should be screened before 48 hours of age.
- A pre-transfusion specimen is essential. If this is impossible, obtain one specimen at 24-48 hours of age and a repeat specimen 3 days after the last transfusion.
- If an initial screen is obtained prior to transfusion when the newborn is older than 24 hours of age, a repeat specimen is not necessary.
- Screening can only be done on neonates/infants not more than 3 months of age utilizing the filter paper cards with the exception of IEM screening (extended screen) can be done on infants or babies.
- Air-dry the filter paper on a flat surface for three to four hours. Do not heat, stack, or allow the blood spots on the filter paper to touch other surfaces during the drying process.
- If specimens cannot be sent for analysis immediately, store them in a plastic bag in a freezer (preferably) or a refrigerator.
CollectionTechnique
The technique for specimen collection is the same as for state-mandated screening programs. The healthcare professional will fill each of the four circles on the filter paper with a single, free-flowing drop of blood. Other important instructions include:
- Do not layer successive drops.
- Apply blood to only one side of the filter paper.
- Make sure the blood has saturated through to the back of the filter paper.
Report: Inborn Errors of Metabolism
- Simplified Report for Amino Acid, Fatty Acid and Organic Acid Disorders.
- Abnormal results may be flagged and information passed to client.
- Referrals may be recommended or follow up testing recommended on a case by case basis. Special follow up tests may be recommended in case of abnormal results.
Chemistry Report
- Special Chemistry and Hormone Tests such as Adrenal hyperplasia.
- Reference Ranges for newborns
Hemoglobinopathy Report
- The Synapse Special Hemoglobinopathy Screen is a comprehensive Genetic Newborn Screen for Hemoglobinopathies which not only detects Sickle cell disease but also Non sickling hemoglobinopathies such as Alpha Thalassemia syndromes (Example: Hb H Disease), Beta Thalassemia syndromes (Example: Hb E/ β 0 thalassemia’s) and Other mutations such as Hb EE Disease.